One therapy with many attributes
POTENT DIFLUORINATED STEROID
With fluorination at the C-6 and C-9 positions1
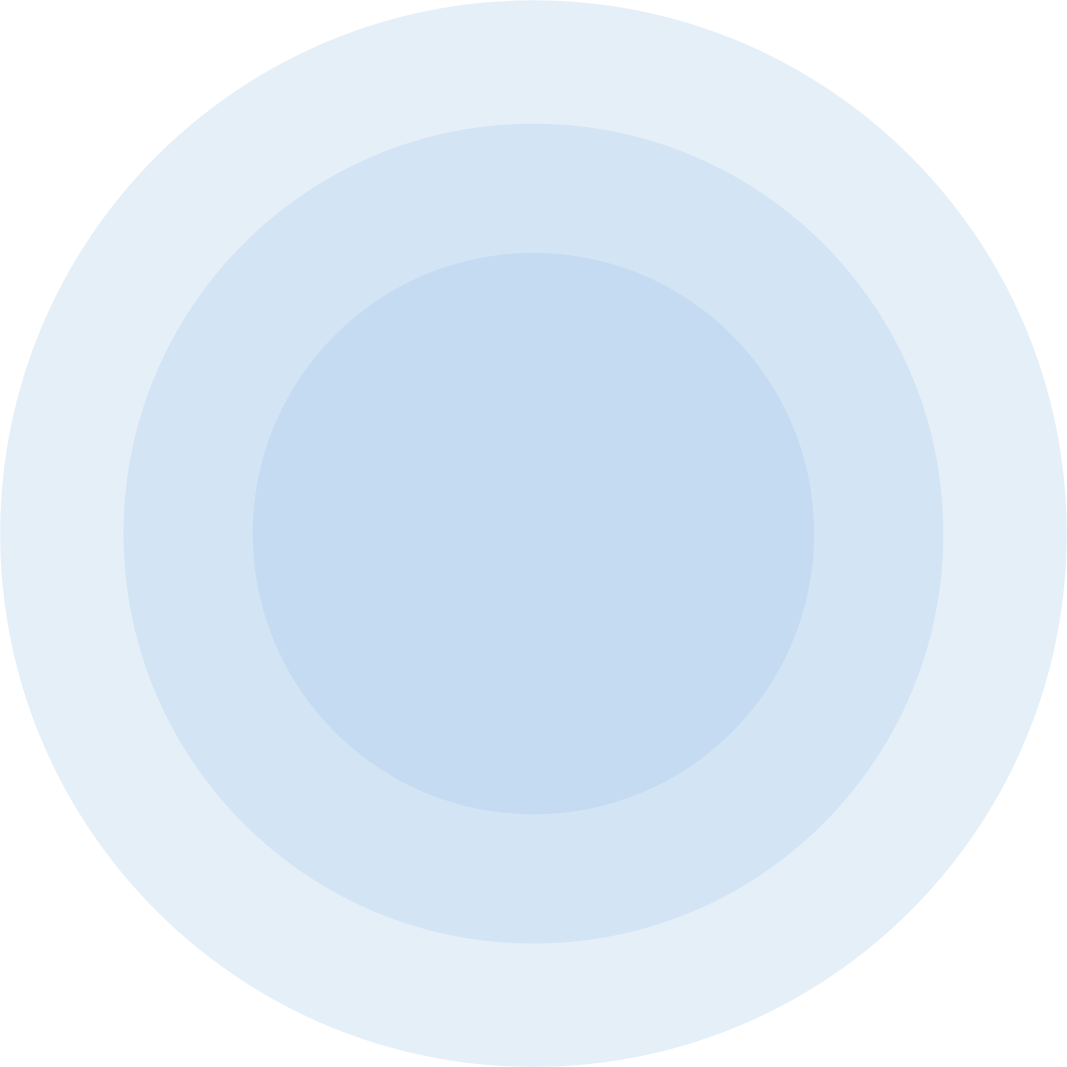
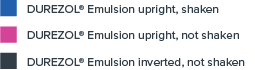
EMULSION FORMULATION FOR DOSE
CONSISTENCY1,10
The only topical ophthalmic steroid formulated as an emulsion, and with proprietary DROP-TAINER® technology1
BAK-FREE TOPICAL OPHTHALMIC STEROID
Preserved with sorbic acid1
CONSISTENT DRUG DELIVERY10
Regardless of bottle orientation or shaking, all DUREZOL® Emulsion concentrations at each time point analyzed were within 15% of declared concentration.10
Percent variation in concentration of active drug dispensed
In clinical studies of cataract surgery patients
Proven to help clear inflammation and resolve ocular pain1
ZERO INFLAMMATION IN NEARLY 3X MORE PATIENTS VERSUS PLACEBO1,11

Percentage of patients with anterior chamber cells clearing (cell count=0)

ZERO PAIN IN NEARLY 2X AS MANY PATIENTS VERSUS PLACEBO1,11

Percentage of patients who were pain free

Help resolve inflammation in patients with endogenous anterior uveitis
For the noninferiority analysis, the upper 95% CL on the difference in mean change from baseline in AC cell grade was required to be <0.5 units. The difference was less than the noninferiority margin at all time points after Day 3.13
Mean change from baseline in AC cell grade13
Study treatment-related ocular adverse events for patients with endogenous anterior uveitis13,14
Study 113
|
Adverse Event |
DUREZOL® Emulsion |
Pred Forte* Suspension |
|---|---|---|
|
Punctate keratitis |
8 (16.0) |
5 (12.5) |
|
Vision blurred |
4 (8.0) |
0 (0.0) |
|
Iridocyclitis |
— |
— |
|
Eye irritation |
5 (10.0) |
1 (2.5) |
|
Dry eye |
3 (6.0) |
0 (0.0) |
|
IOP increase† |
6 (12.0) |
2 (5.0) |
Study 214,15
|
Adverse Event |
DUREZOL® Emulsion |
Pred Forte* Suspension |
|---|---|---|
|
Punctate keratitis |
3 (5.4) |
0 (0.0) |
|
Vision blurred |
1 (1.8) |
0 (0.0) |
|
Iridocyclitis |
3 (5.4) |
2 (3.7) |
|
Eye irritation |
1 (1.8) |
0 (0.0) |
|
Dry eye |
— |
— |
|
IOP increase† |
5 (8.9) |
2 (3.7) |
*Trademark is the property of its owner.
†IOP increases that were reported as an adverse event (which may not have been captured as a “clinically significant IOP rise,” or one that was ≥21 mmHg and change from baseline ≥ 10 mmHg at the same visit).
Safety profile for patients based on ocular surgery clinical trials
Study treatment-related ocular adverse events occurring in more than 2% of patients.1,11
CONJUNCTIVAL HYPEREMIA
DUREZOL®
Emulsion, 4x daily
4.5%
Placebo
19.5%
CILIARY HYPEREMIA
DUREZOL®
Emulsion, 4x daily
4.5%
Placebo
17.3%
ANTERIOR CHAMBER CELL
DUREZOL®
Emulsion, 4x daily
3.6%
Placebo
11.8%
CONJUNCTIVAL EDEMA
DUREZOL®
Emulsion, 4x daily
3.6%
Placebo
6.4%
EYE INFLAMMATION
DUREZOL®
Emulsion, 4x daily
1.8%
Placebo
3.6%
PHOTOPHOBIA
DUREZOL®
Emulsion, 4x daily
3.6%
Placebo
5.5%
PUNCTATE KERATITIS
DUREZOL®
Emulsion, 4x daily
3.6%
Placebo
2.7%
ANTERIOR CHAMBER FLARE
DUREZOL®
Emulsion, 4x daily
0.9%
Placebo
7.3%
IRITIS
DUREZOL®
Emulsion, 4x daily
2.7%
Placebo
0.5%
VISUAL ACUITY REDUCED
DUREZOL®
Emulsion, 4x daily
4.5%
Placebo
8.6%
EYE PAIN
DUREZOL®
Emulsion, 4x daily
5.4%
Placebo
5.0%
FOREIGN BODY SENSATION
DUREZOL®
Emulsion, 4x daily
0.9%
Placebo
4.1%
CORNEAL EDEMA
DUREZOL®
Emulsion, 4x daily
2.7%
Placebo
8.2%
In clinical trials of ocular surgery, the mean IOP in patients receiving DUREZOL® Emulsion did not significantly change and remained in the normal range in all treatment groups11
A clinically significant IOP rise (≥21 mmHg; ≥10 mmHg from baseline) was observed in 3 patients (3%) in the DUREZOL® Emulsion QID group and in 2 patients (1%) in the placebo group.11
When DUREZOL® Emulsion is used for 10 days or longer, IOP should be monitored.1
One patient in the DUREZOL® Emulsion groups and both patients in the placebo group required lOP-lowering medication.11
Prolonged use of corticosteroids may result in glaucoma with damage to the optic nerve and defects in visual acuity and fields of vision. 1

ST-601A-002a and ST-601A-002b
Clinical trial: IOP range11

Observed IOP increase in clinical trials of EAU:
- 6 patients (12%) in the DUREZOL® Emulsion group and 2 patients (5%) in the prednisolone acetate group in Study 113,15
- 5 patients (8.9%) in the DUREZOL® Emulsion group and 2 patients (3.7%) in the prednisolone acetate group in Study 213,15
Proportion of patients with a single-visit change in IOP of ≥10 mmHg from baseline and an observed value of ≥21 mmHg
ST-601A-002a and ST-601A-002b
Clinical trial: IOP Change–DUREZOL® Emulsion vs. Pred Forte*
*Trademark is the property of its owner.
INDICATIONS AND USAGE
DUREZOL® (difluprednate ophthalmic emulsion) 0.05% is a topical corticosteroid that is indicated for:
- The treatment of inflammation and pain associated with ocular surgery.
- The treatment of endogenous anterior uveitis.
Dosage and Administration
- For the treatment of inflammation and pain associated with ocular surgery instill one drop into the conjunctival sac of the affected eye 4 times daily beginning 24 hours after surgery and continuing throughout the first 2 weeks of the postoperative period, followed by 2 times daily for a week and then a taper based on the response.
- For the treatment of endogenous anterior uveitis, install one drop into the conjunctival sac of the affected eye 4 times daily for 14 days followed by tapering as clinically indicated.
IMPORTANT SAFETY INFORMATION
Contraindications
DUREZOL® Emulsion, as with other ophthalmic corticosteroids, is contraindicated in most active viral diseases of the cornea and conjunctiva including epithelial herpes simplex keratitis (dendritic keratitis), vaccinia, and varicella, and also in mycobacterial infection of the eye and fungal diseases of ocular structures.
Warnings and Precautions
- Intraocular pressure (IOP) increase – Prolonged use of corticosteroids may result in glaucoma with damage to the optic nerve, defects in visual acuity and fields of vision. If this product is used for 10 days or longer, IOP should be monitored.
- Cataracts – Use of corticosteroids may result in posterior subcapsular cataract formation.
- Delayed healing – The use of steroids after cataract surgery may delay healing and increase the incidence of bleb formation. In those diseases causing thinning of the cornea or sclera, perforations have been known to occur with the use of topical steroids. The initial prescription and renewal of the medication order beyond 28 days should be made by a physician only after examination of the patient with the aid of magnification such as slit lamp biomicroscopy and, where appropriate, fluorescein staining.
- Bacterial infections – Prolonged use of corticosteroids may suppress the host response and thus increase the hazard of secondary ocular infections. In acute purulent conditions, steroids may mask infection or enhance existing infection. If signs and symptoms fail to improve after 2 days, the patient should be re-evaluated.
- Viral infections – Employment of a corticosteroid medication in the treatment of patients with a history of herpes simplex requires great caution. Use of ocular steroids may prolong the course and may exacerbate the severity of many viral infections of the eye (including herpes simplex).
- Fungal infections – Fungal infections of the cornea are particularly prone to develop coincidentally with long-term local steroid application. Fungus invasion must be considered in any persistent corneal ulceration where a steroid has been used or is in use.
- Contact lens wear – DUREZOL® Emulsion should not be instilled while wearing contact lenses. Remove contact lenses prior to instillation of DUREZOL® Emulsion. The preservative in DUREZOL® Emulsion may be absorbed by soft contact lenses. Lenses may be reinserted after 10 minutes following administration of DUREZOL® Emulsion.
Most Common Adverse Reactions
- In postoperative ocular inflammation and pain studies, ocular adverse reactions occurring in 5-15% of subjects included corneal edema, ciliary and conjunctival hyperemia, eye pain, photophobia, posterior capsule opacification, anterior chamber cells, anterior chamber flare, conjunctival edema, and blepharitis.
- In the endogenous anterior uveitis studies, the most common adverse reactions occurring in 5-10% of subjects included blurred vision, eye irritation, eye pain, headache, increased IOP, iritis, limbal and conjunctival hyperemia, punctate keratitis, and uveitis.
For additional information about DUREZOL® Emulsion, please see full Prescribing Information.
References: 1. Durezol [package insert]. Fort Worth, TX: Alcon Laboratories, Inc; April 2017. 2. US Food and Drug Administration. Orange book: approved drug products with therapeutic equivalence evaluations. https://www.accessdata.fda.gov/scripts/cder/ob/results_product.cfm?Appl-Type=N&Appl_No=022212. Updated October 2015. Accessed December 15, 2015. 3. Alrex [package insert]. Bridgewater, NJ: Bausch & Lomb Inc; 2016. 4. FML [package insert]. Irvine, CA: Allergan Inc; 2013. 5. Lotemax Gel [package insert]. Bridgewater, NJ: Bausch & Lomb Inc; 2016. 6. Lotemax Suspension [package insert]. Bridgewater, NJ: Bausch & Lomb Inc; 2016. 7. Maxidex [package insert]. Fort Worth, TX: Alcon Laboratories Inc; 2002. 8. Pred Forte [package insert]. Irvine, CA: Allergan Inc; 2017. 9. Vexol [package insert]. Fort Worth, TX: Alcon Laboratories Inc; 2012. 10. Stringer W, Bryant R. Dose uniformity of topical corticosteroid preparations: difluprednate ophthalmic emulsion 0.05% versus branded and generic prednisolone acetate ophthalmic suspension 1%. Clin Ophthalmol. 2010;4:1119-1124. 11. Korenfeld MS, Silverstein SM, Cooke DL, Vogel R, Crockett RS; Difluprednate Ophthalmic Emulsion 0.05% (Durezol) Study Group. Difluprednate ophthalmic emulsion 0.05% for postoperative inflammation and pain. J Cataract Refract Surg. 2009;35(1):26-34. 12. Data on file. 13. Foster CS, DaVanzo R, Flynn TE, McLeod K, Vogel R, Crockett RS. Durezol® (difluprednate ophthalmic emulsion 0.05%) compared with Pred Forte® 1% ophthalmic suspension in the treatment of endogenous anterior uveitis. J Ocul Pharmacol Ther. 2010;26(5):475-483. 14. Sheppard JD, Toyos MM, Kempen JH, Kaur P, Foster CS. Difluprednate 0.05% versus prednisolone acetate 1% for endogenous anterior uveitis: a phase III, multicenter, randomized study. Invest Ophthalmol Vis Sci. 2014;55(5):2993-3002. 15. Data on file.